Megan Hyun, PhD

Research interests
Adaptive radiotherapy (ART): Conventionally, radiation therapy treatment plans are created with sufficient margins for the same plan to be delivered each day of treatment, despite patient setup uncertainties, internal anatomic variation, and changes in body habitus. Interest has increased over the past 20 years in adapting the patient's treatment plan as these changes are observed, but there are substantial technological limitations preventing large clinical trials and widespread clinical adoption. Our aim is to pave the way for clinical trials and more widespread use of ART by developing and implementing simple, offline adaptive workflows that can be used at many clinics, and to overcome some of the challenges in deformable image registration seen for sites like prostate.
Education innovation and research: We aim to elevate educational standards in medical physics teaching through innovation and educational scholarship at multiple levels, including radiation therapy students, graduate students, residents, practicing physicists, patients, and the public. Projects have included interactive laboratory exercises in a virtual linac environment ("Vert"), flipped-classroom approaches, rigorous clinical procedure training, and engaging eLearning modules. Our current emphasis is teaching physicists how to interact with patients through the development of a novel training program combining eLearning with in-person simulation-based learning. In each of these projects, we aim to evaluate the efficacy of teaching interventions so the knowledge we gain can benefit the larger medical physics community.
Bioethics and medical physics: As new technologies such as AI are introduced in medicine generally, and radiation oncology in particular, the need for collaborations between medical physics and bioethics becomes more apparent. Can physicist-patient consultations help us respect patient autonomy to a greater degree? What are the ethical dangers of implementing artificial intelligence tools in the clinic, when they may have been developed with limited datasets? In a unique collaboration between philosophy and medical physics, we apply technical expertise and logical rigor to answering hard questions like these.
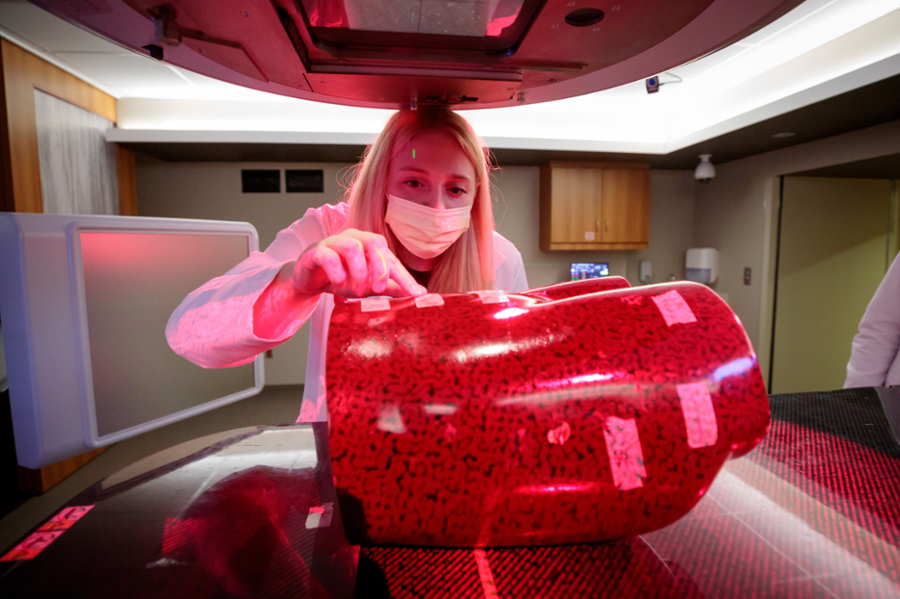
Radiation dosimetry: Accurate dose determination can be challenging under nonstandard conditions such as small fields, ultra-high dose rates (e.g., FLASH), and targeted radionuclide therapy. We apply rigorous measurement and calculation techniques to determine correction factors and models necessary for the most accurate dose estimation under these and other nonstandard conditions.