When we’re driving to a new destination, we often turn down the stereo as we follow the directions. What had been music suddenly sounds like noise, and it interferes with our focus.
Our understanding of how infectious diseases like COVID affect human lungs has been similarly confounded by noise. Data from patient lung tissues greatly varies from person to person, obscuring the basic mechanisms of how, exactly, SARS-Co-V2 first infects lung cells. It’s also an after-the-fact analysis—as if we’re trying to map the route the virus took three states back.
Turning down the noise of variability by studying genetically identical tissues from the first moment of infection could light up the route the pathogen takes. Which cells are infected, and when? What is the level of infection, and how does it differ depending on cell type? How does it change in different conditions?
And what if it were possible to track thousands of these infections at once? It might revolutionize our understanding of both infections and the drug treatments used to combat them.
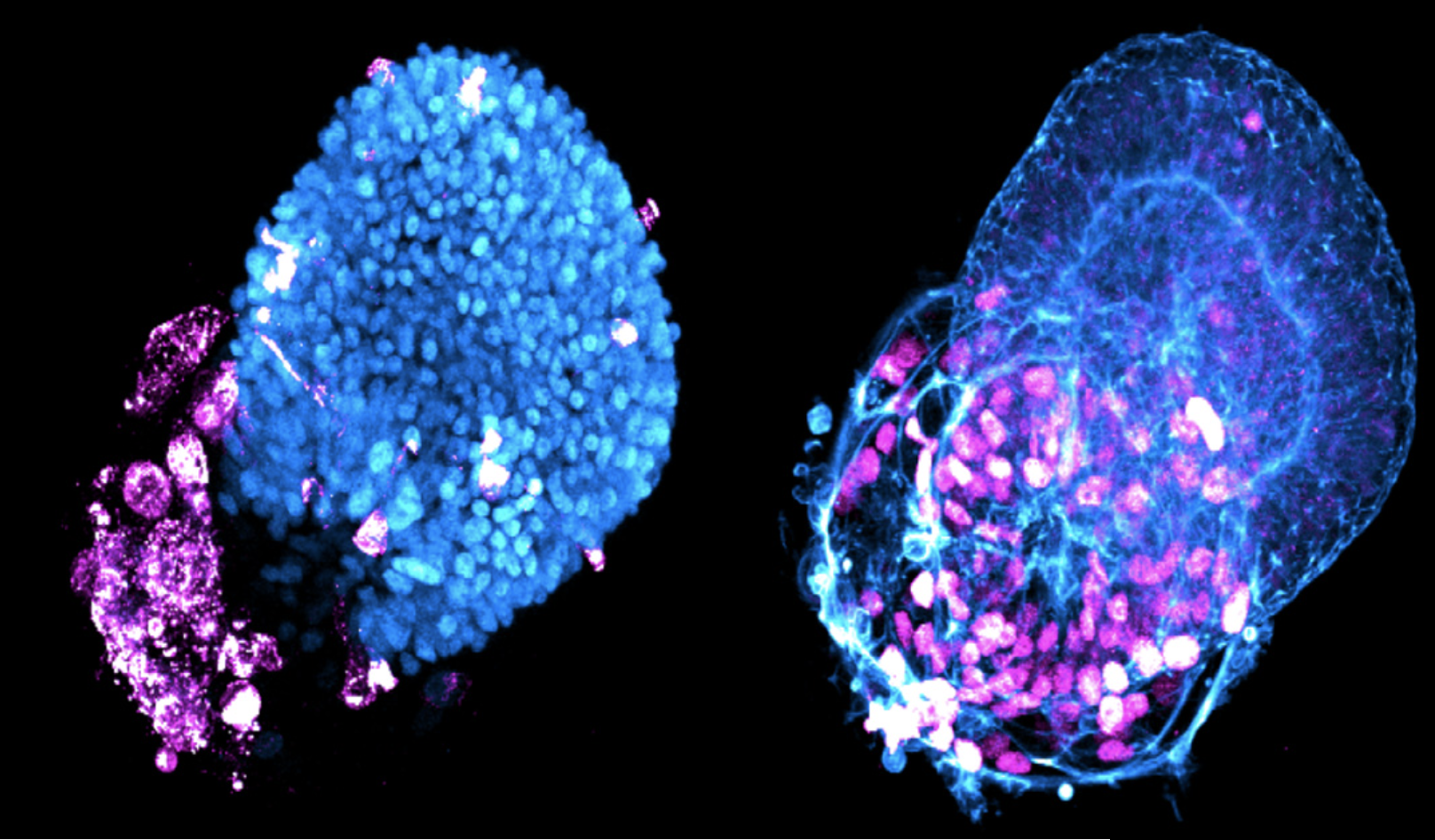
That’s the hope for new advanced tech capable of growing mini organs on microchips. The labs of Rockefeller’s Ali Brivanlou and Charles M. Rice collaborated to refine a cell culture technology platform that grows genetically identical lung buds—the embryonic structures that give rise to our breathing organs—from human embryonic stem cells (hESCs). Their findings were recently published in Stem Cell Reports.