Marilynn A. Larson, M.Sc., PhD
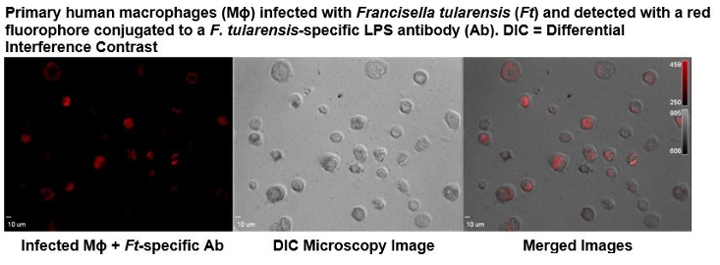
Dr. Larson’s research is focused on elucidating the molecular mechanisms that allow intracellular pathogens to evade the immune system and persist. These assessments include the use of Francisella tularensis as a model system, since considerable differences in virulence exist between the subpopulations in this species, including select agents, attenuated strains, and avirulent strains. This facultative intracellular bacterium is the etiologic agent of the zoonotic disease tularemia, in which there is no effective vaccine. The highly infective strains are among the most pathogenic bacteria known with the potential to be used as a bioweapon and therefore, are classified as Tier 1 select agents by the Centers of Disease Control and Prevention. Although the genome of the type A.I, A.lI, and B clades within this species share 98% average nucleotide identity, insertion sequence elements have contributed to numerous chromosomal rearrangements between these subpopulations. The resulting changes in gene expression from these translocations, as well as other polymorphisms are being examined using a systems biology approach. These evaluations include the study of host-pathogen interactions elicited during a human macrophage infection. Together these investigations will provide a better understanding of the multifactorial mechanisms utilized by the highly virulent F. tularensis A.I strains, which enhances pathogenicity, and contribute to the development of effective countermeasures against F. tularensis and other intracellular pathogens. Additional research projects include the development of next generation molecular diagnostics for select agent and clinical pathogen identification and characterization, the detection of stable biomarkers that are indicative of an infection or radiation exposure, and the discovery of therapeutics to prevent or treat infections. Dr. Larson's research is also listed under High Risk Organisms and Host-pathogen Interactions.
Joshua L. Santarpia, PhD
Aerosol Transmission of Disease: Dr. Santarpia’s lab works to understand the role of aerosols in the transmission of disease. In particular his lab has worked to develop an understanding of the role aerosols play in the transmission of SARS-CoV-2 and to characterize the transport of aerosol in built environments such as hospitals, schools, work environments and transportation.
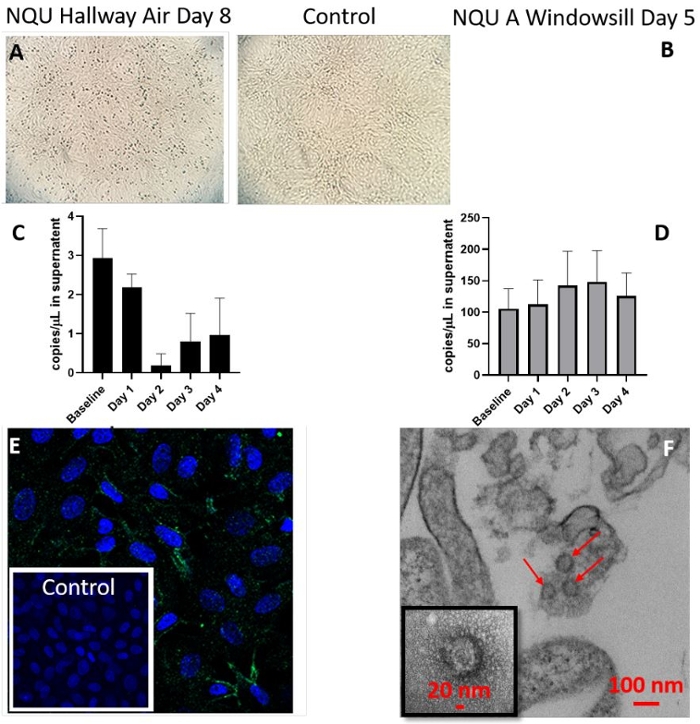
Results of SARS-CoV-2 cell culture experiments. Images and graph describe the results of cell culture of two environmental samples. The two samples are shown: an air sample from the NQU hallway on day 8 (A,C, and E), the windowsill from NQU A on day 1 (B,D, and F). Cytopathic effect observed in these samples (A-B) is generally mild, compared to the control (top center) which had no environmental sample added. RT-qPCR from daily withdrawals of 100 µL of supernatant from the cell culture of each sample indicates changes in viral RNA in the supernatant throughout cultivation. The hallway air sample indicates a decrease in RNA concentration in the supernatant over the first 2 days, consistent with the withdrawal of supernatant for analysis. Increase in concentration is observed on both days 3 and 4 (C). The windowsill sample showed stable and possible increasing viral concentrations for the first 3 days, despite the withdrawal of supernatant for analysis (D). Immunofluorescent staining of the hallway air sample indicates the presence of SARS-CoV-2, after 3 days of cell culture (E), as compared to control cells (inset), which were not exposed to any environmental sample. TEM images of the lysates from the windowsill culture (F) clearly indicate the presence of intact SARS-CoV-2 virions, after 3 days of cell culture.

