 |
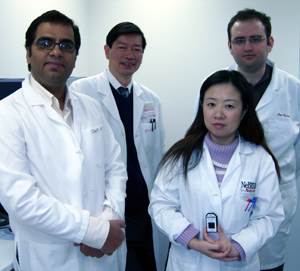
John Chan, M.D., principal investigator of a study published Nov. 27 in the New England Journal of Medicine, second from left, with part of his research team. Others from the left are Javeed Iqbal, Ph.D., Zhong Feng Liu, M.D., and Can Kucuk. Dr. Liu holds a gene chip that stores information about a patient’s lymphoma that is used to perform DNA microarray analysis. |
The information may be critical in tailoring cancer treatment in the near future.
“There have been a number of reports saying that gene expression profiling of diffuse large B cell lymphoma is no longer important with current treatment. But we found that it still does predict survival for this type of lymphoma,” said John Chan, M.D., Amelia and Austin Vickery Professor of Pathology, co-director of the UNMC Center for Lymphoma and Leukemia Research and principal investigator of the study.
Dr. Chan and Louis Staudt, M.D., Ph.D., of the National Cancer Institute, are co-senior authors of the paper.
In 2002, a consortium of eight institutions around the world published groundbreaking information about the role of gene expression profiling using sophisticated DNA microarray technology.
The information revealed that diffuse large B cell lymphoma actually is two distinct diseases and should be treated as such. At the time, diffuse large B cell lymphoma was treated with CHOP — a chemotherapy regimen. Since then, a better treatment regimen was discovered — CHOP plus an additional antibody, Rituximab — called R-CHOP.
Because survival rates have improved significantly with R-CHOP treatment, Dr. Chan said many oncologists felt that a predictor of survival — defined by gene expression profiling — may no longer hold value as a guide for treatment.
The goal of the study was to see if their model for prognosis developed in 2002 was still valid.
When researchers re-evaluated patients treated with R-CHOP, they found their original predictors are still valid. Patients with a type of diffuse large B-cell lymphoma called germinal center B-cell-like who were treated with R-CHOP had a more favorable survival than those with an activated B-cell-like diffuse large B cell lymphoma, with three-year overall survival rates of 84 percent and 56 percent, respectively.
Researchers concluded that survival following treatment of diffuse large B-cell lymphoma is influenced not just by the advanced R-CHOP treatment, but also by differences in the tumor.
“Rituximab improves survival for both types of diffuse large B cell lymphoma, but still the differential in prognosis using gene expression profiling is valid,” Dr. Chan said. “The study is significant in the sense that we redefined prognosticators for current therapy and dispelled the erroneous belief that has come up during the past few years.”
|
|
Julie Vose, M.D., UNMC chief of the section of hematology/oncology, who also collaborated in the research, said the paper is very important.
“This paper confirms that the model currently used still is significant in benefitting patients,” Dr. Vose said. “We still need to target improved therapy for patients.”
Dr. Vose is involved in the first clinical study that recently was launched at UNMC to test the research model in patients. The pilot study will evaluate 40 patients. If successful, a larger, national study will be conducted.
She said in the next five to 10 years, the information could be useful to oncologists in tailoring treatment.
In addition, oncologists may consider doing transplants earlier in patients with poor prognosis or they might treat patients more aggressively with closer intervals of treatment.
Dr. Chan said the study also revealed information about the significance of the tumor environment.
“The genetic makeup of the tumor cell affects survival. The host reaction to the tumor is also very important, and this can be assessed by measuring the expression of a group of genes reflecting the tumor microenvironment — the stromal signature,” Dr. Chan said. “We found that this stromal signature can be split into two components. High expression of one of them is associated with good prognosis while high expression of the other one is associated with poor prognosis.”
The consortium has published about 30 papers on gene expression profiling of lymphoma since 1999. A 2003 paper published in the Journal of Experimental Medicine further identified a third and distinct type of diffuse large B cell lymphoma. In addition to germinal center B-cell-like and activated B-cell-like, researchers identified a subtype called primary mediastinal B-cell lymphoma that generally has favorable outcome.
Other UNMC authors on the paper were Dr. Vose, Javeed Iqbal, Ph.D., Martin Bast, Kai Fu, M.D., Ph.D., Dennis Weisenburger, M.D., Timothy Greiner, M.D., and James Armitage, M.D.