It’s just a small molecule, but it has the potential to predict if coronary artery disease is in your future.
Or rheumatoid arthritis (RA).
Or diabetes.
Or a multitude of other diseases, all due to the level of inflammation.
It’s called the malondialdehyde-acetaldehyd adduct (MAA), which Geoff Thiele, Ph.D., a professor of internal medicine, began studying in 1996 to better understand its relationship with alcoholic liver disease and hepatitis.
Recently, he and Ted Mikuls, M.D., professor, rheumatology, noticed that the presence of antibodies to MAA, was linked to high levels of inflammation in patients with RA. As a result, they developed a test that determines whether a patient is harboring increased levels of these antibodies to MAA.
“It’s the ultimate pan-marker – an indication of inflammation in any disease process,” Dr. Thiele said. “Using this test, the physician may gain insights into the level of inflammation that is occurring over time as well as possible co-morbidities associated with RA. Now, we’re looking at whether the antibodies to MAA can aid in the prediction of cardiovascular disease.”
The team began an interdisciplinary collaboration with Dan Anderson, M.D., Ph.D., assistant professor in cardiology, who has a frontline view of the battle against the world’s most prolific killer.
“We know that inflammation is important in cardiovascular disease,” Dr. Anderson said. “But we don’t understand a lot about why or how.
“To be alive is to be inflamed, and it’s when cells are stressed with high cholesterol, RA or diabetes that they create high MAA and anti-MAA levels.”
But imagine a test that could both predict these diseases years before they manifest and advance preventive medicine, saving millions of lives and dollars.
Right now in the U.S.:
- Nearly everyone over age 50 – more than 98 million Americans – has some level of coronary artery disease. So do 70 percent of 40-year-olds. About one-half of people in their 20s and 30s probably have it too.
- Cardiovascular disease causes about 2,200 deaths a day, averaging one death every 40 seconds. The annual direct and indirect costs of cardiovascular disease and stroke are about $315 billion.
- 52.5 million suffer from arthritis; 1.3 million have rheumatoid arthritis. Americans pay $39.2 billion a year in direct, indirect and intangible costs for this No. 1 cause of disability in the country.
- 50 million individuals suffer from autoimmune disease. The annual direct health care cost is $200 billion.
Ted Mikuls, M.D., Geoff Thiele, Ph.D., and Dan Anderson, M.D., Ph.D., research ways to use MAA as a predictor for rheumatoid arthritis and heart disease.
Dr. Anderson envisions this test being part of the normal blood panel.
“The ideal test would be to draw blood from young patients and follow them. We could predict from initial blood work who would develop any of these diseases later in life,” he said.
By current measures, Dr. Anderson said, about 30 percent of people with heart disease slip through the cracks. Too often, the first indication of trouble may be a killer heart attack.
But others with the disease suffer few, if any, ill-effects. Predicting which patients will develop the deadlier form of heart disease is little more than a guess.
“From a clinical diagnostic perspective, this becomes invaluable to help understand those different groups of patients,” Dr. Anderson said.
Dr. Thiele said he hit a dead end studying alcoholic liver disease in humans. First, in this disease the animal models simply do not mimic the disease. Secondly, it was difficult to get liver samples from patients early in the course of alcoholic hepatitis. Finally, there is no current reliable biomarker to use in following these patients. But he did notice that wherever there was inflammation, high levels of MAA and anti-MAA antibodies were present.
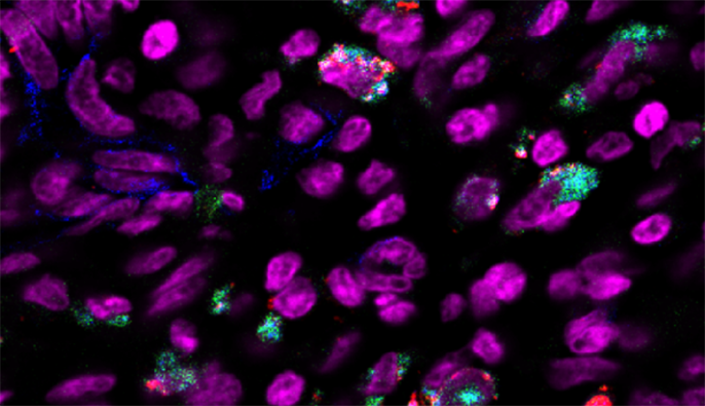
MAA is produced during inflammation to bind to proteins in your body. Normally, our immune system does not react to our own proteins. “We have shown that when proteins are modified with MAA, the immune system sees these as foreign. The immune system produces antibodies and T-cells to MAA and to the proteins to which it is attached and begins to attack.”
“This little molecule holds a lot of promise.”
Geoff Thiele, Ph.D.
The problem now is to identify which protein is related to which disease. The answers may rest within the dozen or so biobanks of tissue and blood at UNMC and around the country that provide him with more than enough research samples. “I walked into a gold mine when I started working with Dan and Ted,” he said.
His collaboration with Drs. Anderson and Mikuls has opened his research to several national studies including one with Harvard University. Now, MAA is linked to new studies of oxidative stress and aneurisms.
The research team and UNMC’s technology transfer office, UNeMed Corporation, are working with Chinese scientists to replicate Dr. Thiele’s study to apply it to atherosclerosis disease, which is closely linked to stroke – the fourth leading cause of death in China.
UNeMed also is looking for entrepreneurs to start a company that will conduct trials to further validate the MAA adduct and antibodies to MAA, and then seek a partner to license the patents of the diagnostic marker.
The next round of testing will be critical to understand how accurate the test can be, particularly studies that follow individual patients over the course of five or 10 years, Dr. Thiele said.
“This little molecule holds a lot of promise.”