Beginning Wednesday, April 15, Nebraska Medical Center will use a new device, called an Infectious Aerosol Capture Mask (IACM), to capture exhaled aerosolized particles at their source from patients.
Approved by the Nebraska Medicine Innovation Committee, the hospital plans to initially deploy the IACM, developed by Steven Lisco, MD, chair of the UNMC Department of Anesthesiology, in the operating room for use with patients who aren’t showing symptoms of COVID-19, but may or may not have the disease. This device will be used on patients who are undergoing monitored anesthesia care and will be used during and after emergence from general endotracheal anesthesia, as well as in the post-anesthesia care unit. If successful in this environment, the IACM could also be used for patients confirmed to have COVID-19 and are receiving care in the ICU or emergency department.
Patients with COVID-19 produce microscopic aerosol particles, which fill the patient’s environment and increase the risk of disease transmission. A small percentage of patients also may produce aerosols when not showing symptoms or before showing symptoms.
These patients are a challenge for providers, as they may unknowingly produce infectious aerosols when coughing, wearing supplemental oxygen or undergoing aerosol-generating procedures like intubation and extubation – all common occurrences in operating rooms and in post-anesthesia care units.
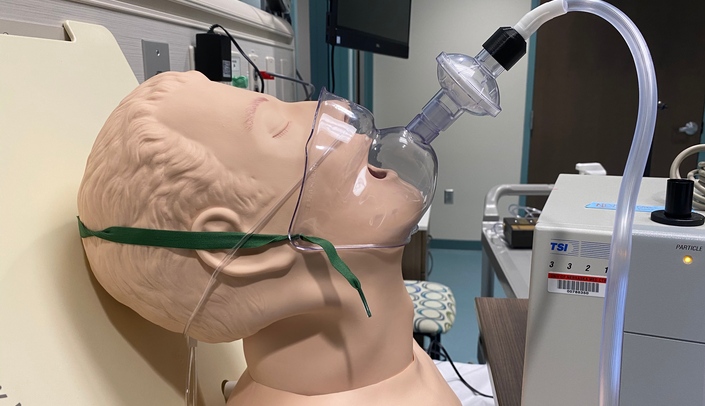
The IACM device uses a face tent (shown in attached pictures), positioned upside down with a viral filter attached, connected to wall suction. The apparatus attaches to the vacuum source via standard suction tubing adapted to the device via a plastic piece created with a 3D printer by Nicholas Markin, MD, director of perioperative imaging.
“The IACM performed very well in laboratory testing in conjunction with a nasal device used to deliver supplemental oxygen, catching more than 90% of airborne particles expelled in the mask, ultimately preventing the aerosol from entering the patient environment,” says Dr. Lisco. “Even when the vacuum wasn’t turned on, the mask was still 85% effective as a barrier.”
Dr. Lisco adds that in these areas, patients are often given nasal cannula oxygen, which has been shown to increase the rate and density of aerosolized particles.
“Additionally, work in these areas often mandates that patients and health care workers be in close proximity,” says Dr. Lisco. “While risk of infection transmission is extremely low, efforts to reduce environmental aerosol contamination are still justified.”
According to Dr. Lisco, using this device with COVID-19-positive patients who require supplemental oxygen also will be beneficial for reducing health care worker risk in the intensive care unit.”
“We think it is far superior to put this device on patients in the PACU or ICU versus a surgical mask over a nasal oxygen delivery device,” says Dr. Lisco. “This is a game of inches, and we’re in the red zone. We will do anything we can do protect our health care workers and our community.”