 |
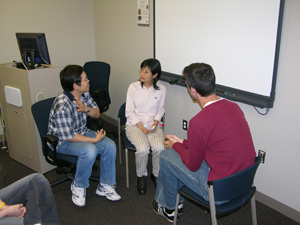
Medical student Eric Schneider (right) listens as Xingqi Wang (left) translates for Jianhong Sun. The UNMC employees, who speak Chinese, volunteered to help students learn how to effectively use interpreters in medical settings. |
Even then, there’s an art to producing an effective patient/interpreter experience.
For the past 14 years, second-year medical students at UNMC have gotten a taste of working with professional and non-professional interpreters and non-English speaking patients to better understand how to overcome communication barriers.
In the mock sessions held earlier this month, second-year student Jessica Moran met with a German-speaking man suffering from stomach cramps.
Student Ari Nowacek spoke with a Chinese-speaking woman complaining of shoulder pain.
During the Integrated Clinical Experience (I.C.E.) curriculum, fellow classmates met with other simulated patients who spoke only Hindi, French, Vietnamese, Korean and Spanish.
In each case, a non-professional interpreter facilitated the exchange of information.
“The culture is changing and becoming more diverse, even in Nebraska,” Dr. Flores said. “There will be a time in every physician’s life where they’ll need an interpreter, so we want to teach them the right way to do it and be most effective. You can have an interpreter in the room and still have an inefficient patient/interpreter experience.”
Each year, the UNMC College of Medicine recruits pairs of people who speak a second language or do sign language for the small group sessions. The volunteers are given fictitious medical conditions to share with the students through an interpreter. The student, in turn, relates their questions and diagnosis through the interpreter.
In doing so, students discover how to effectively use a translator by:
- Using shorter sentences than normal – they’re easier for the interpreter to translate and better understood by the patient.
- Reading a patient’s body language and facial expressions to gauge whether they understand what is being said.
- Talking and looking at the patient, not the interpreter, during the visit.
- Asking the interpreter for a full and complete translation, especially if the interpreter responds briefly after a patient has spoken at length.
- Positioning the patient and interpreter so everyone can easily see each other.
- Using simple terminology the patient can understand.
“I see a lot of Sudanese patients, so going through the experience in 1998 was really beneficial to me,” said Dr. Flores, a 2001 UNMC graduate. “There’s more to communication than the spoken word and interpreters can help provide insight into another culture.”
 |
UNMC medical student Jessica Moran (right) doesn’t speak German, so Cora Connor interprets for ‘patient’ Reece Conner in a mock clinical setting. |
In December 2000, the U.S. Office of Health and Human Service Office of Minority Health published the Culturally and Linguistically Appropriate Services (CLAS) standards to help eliminate racial and ethnic health disparities. One of the mandates requires health care organizations to offer and provide language assistant services at no cost to each patient with limited English proficiency.