 |
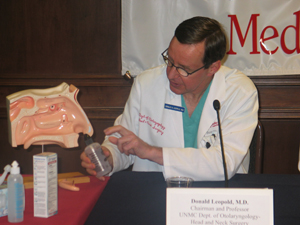
Donald Leopold, M.D., demonstrates the use of a saline nasal rinse that he says in many cases should be used over antibiotics to treat sinus infections. Dr. Leopold, professor and chairman of the UNMC Department of Otolaryngology-Head and Neck Surgery, contributed to a study that showed U.S. physicians may be overprescribing antibiotics for sinus infections. |
The study shows U.S. physicians prescribe antibiotics for nearly 83 percent of acute sinus infections and roughly 70 percent of chronic sinus infections, despite viruses, not bacteria, being the most frequent cause of these conditions. Viruses are not affected by antibiotics. The impact of the study is large because an estimated 20 percent of adults and 10 percent of children currently on antibiotics take them for sinus infections.
Hadley Sharp, lead author of the paper, and colleagues in the UNMC Department of Otolaryngology-Head and Neck Surgery, used data from two national surveys to assess the medications prescribed for sinus infections at physicians’ offices and hospital outpatient and emergency departments between 1999 and 2002. The surveys were conducted by the National Center for Health Statistics and designed to be representative of the U.S. population.
“When two-thirds of patients with sinus symptoms expect or receive an antibiotic and as many as one-fifth of antibiotic prescriptions for adults are written for a drug to treat rhinosinusitis, these disorders hold special pertinence on the topic,” said Sharp, a senior medical student. “While keeping the goals of treatment in mind, there are concerns about the overuse of antibiotics and the resultant problems, including drug resistance and increasingly virulent bacteria.”
Co-authors are Donald Leopold, M.D., professor and chairman of the UNMC Department of Otolaryngology-Head and Neck Surgery, David Denman, M.D., an Omaha ENT specialist, and Susan Puumala, formerly of UNMC Preventive and Societal Medicine.
Rhinosinusitis, commonly referred to as a sinus infection, is an inflammation of the sinus cavities that are adjacent to the nasal passages.
It is a common and expensive medical condition in the United States. Based on the data collected in the surveys, an estimated 14.2 million visits to health care facilities nationally per year were due to chronic rhinosinusitis and 3.1 million were because of acute rhinosinusitis.
While antibiotics don’t effectively combat viral sinus infections, they do work in treating infections caused by bacteria. Physicians say treating sinus infections is difficult because there are limited medications on the market for the condition and it is difficult to determine if the patient has an infection caused by bacteria or virus.
Those who suffer from sinus infections seek relief for symptoms such as blocked nasal airflow, mucus, pressure and pain in the sinus areas.
Infection is considered acute when symptoms last up to four weeks and chronic when symptoms persist for 12 weeks or longer. Acute rhinosinusitis is more commonly caused by infectious agents, while allergies, facial anatomy and hormonal changes may contribute to chronic cases.
The most frequently recommended medications for treatment of both acute and chronic rhinosinusitis are antibiotic agents, followed by antihistamines, nasal decongestants, corticosteroids and antitussive, expectorant and mucolytic agents, respectively, the authors wrote.
 |
From left: Donald Leopold, M.D., senior medical student Hadley Sharp and David Denman, M.D., an Omaha ENT specialist, discuss a study they conducted that shows physicians may be overprescribing antibiotics for sinus infections. Sharp served as lead author for the report that notes many sinus infections are caused by viruses, which are not affected by antibiotics. |
Watchful waiting, saline rinse and use of a decongestant or appropriate antimicrobial agents are the preferred treatments, Dr. Leopold said.
“The data in our study says physicians aren’t following the suggested guidelines for treating sinus infections,” Dr. Leopold said. “We want to discourage physicians from prescribing antibiotics too often, ask patients not to inappropriately seek antibiotics and suggest looking at alternative treatments.”
It is possible that physicians may have been treating secondary infections with antibiotics in some cases, the authors note. In addition, physicians may believe that antibiotics are effective because patients improved while taking them, while in fact the symptoms may have cleared up without treatment.
|
|
With few medications to choose from and patients pushing their doctors for relief, many physicians probably feel pressured to prescribe antibiotics.
Dr. Leopold suggests another option that appears to be more effective and less costly than antibiotics: saline irrigation.
“That, for me, has for many years been my main mode of therapy and I don’t think the message is getting down to primary care physicians,” he said. “I would suggest for someone with acute symptoms, viral or bacterial, treating with saline lavage (rinse) is the very best thing.”
Saline rinsing can make symptoms go away, reduce inflammation, rid nasal passages of stagnant mucous and flush the nasal system — making it difficult for opportunistic infections to develop, Dr. Leopold said.