 |
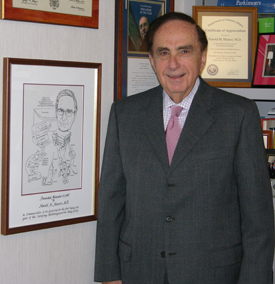
UNMC Chancellor Harold M. Maurer, M.D., with a caricature drawing given to him by members of the Intergroup Rhabdomyosarcoma Study Group, which Dr. Maurer headed for 25 years. The group’s research recently was lauded by the National Cancer Institute, which proclaimed the group’s work to be among the major milestones in the history of pediatric oncology. |
What most people don’t realize about Dr. Maurer is that he was a prolific researcher prior to coming to UNMC and is considered a legendary figure in pediatric oncology.
His legend status was reaffirmed last month when the National Cancer Institute devoted the entire issue of its NCI Cancer Bulletin electronic newsletter to pediatric oncology. The special issue included 12 separate articles dealing with pediatric oncology, including a listing of 28 milestones over the past 60 years in pediatric oncology. The newsletter can be found by clicking here.
One of the milestones during the 1970s was the work of the Intergroup Rhabdomyosarcoma Study Group (IRSG) headed by Dr. Maurer. The IRSG was credited with developing a repetitive-course, multi-agent chemotherapy treatment for advanced rhabdomyosarcoma, a fast-growing, highly malignant tumor that accounts for more than half of the soft tissue cancers in children.
The work of the IRSG is credited with raising the cure rate of children afflicted with the disease from 20 percent to 75 percent.
“It’s very satisfying to see the IRSG’s work be recognized as a milestone in pediatric oncology,” Dr. Maurer said. “It was a real team effort … a lot of good people working together.”
Dr. Maurer’s involvement with rhabdomyosarcoma was somewhat serendipitous.
“I was a new faculty member in 1968 at the Medical College of Virginia in Richmond,” he said. “I was working with Dr. Clare Shumway (a pediatric oncologist/hematologist). He would get depressed every time a child would come in with cancer. Finally, he told me, ‘You do the oncology cases. I’ll take care of the hematology cases.'”
Soon thereafter, a young girl presented to Dr. Maurer with rhabdomyosarcoma. “She had a primary tumor in her leg, and it had metastasized to the lung,” he said. “I checked the medical literature, but there was nothing of any importance that had been written on rhabdomyosarcoma.”
Fortunately, the girl survived. But, Dr. Maurer knew that something needed to be done so that physicians would know how to better treat the disease.
“I met with Dr. Lucius Sinks (director of pediatrics at Roswell Park Cancer Institute in Buffalo, N.Y.), who was head of the Cancer and Leukemia Group B pediatric research consortium at the time,” he said. “He suggested that I go ahead and prepare a research plan and try to pull together other children’s cancer study groups.”
Dr. Maurer was ecstatic. “When I came home, I told (his wife) Beverly: ‘What an opportunity! This is the chance of a lifetime. I’m going to become an expert on rhabdomyosarcoma, and I’ll be able to do something special.'”
The IRSG was soon formed with Dr. Maurer serving as chairman. It included pediatric oncologists from three study groups — Cancer and Leukemia Group B, the Southwest Oncology Group and the Children’s Cancer Study Group.
The oncologists pooled all their rhabdomyosarcoma cases so they could compare outcomes and the treatments that were delivered. The IRSG met four times a year and soon received funding from the National Institutes of Health.
“We needed to do a better job of studying rhabdomyosarcoma. We had to find out how it spreads and where it occurs, then come up with a protocol for treating it,” he said. “We wanted more cases to review, so we even contacted oncologists in the United Kingdom, Germany, Italy and France. We tried to compare our research with their’s.
“We published papers like crazy. We developed common definitions and a classification system with universal groupings of patients. We took it apart. It was a lot of fun.”
Soon, people started to take notice. “I was getting three to five calls a day from physicians around the world seeking my counsel on rhabdomyosarcoma,” he said. Among the callers was the physician for the Amir of Qatar, whose son had the disease.
 |
Dr. Maurer points to a picture of young cancer patients he helped during his time with the Intergroup Rhabdomyosarcoma Study Group. To the right of the picture is a graph that illustrates the drastic increase in survival rates of children with rhabdomyosarcoma during Dr. Maurer’s time leading the group. |
“I told them to send me the slides,” Dr. Maurer said. “This was on a Thursday. By the next Tuesday — thanks to the assistance of the local Air Force Base — we had the slides.
“When I reviewed the slides, I could tell immediately it was a dental problem (necrotizing granuloma), not a rhabdomyosarcoma. I told them ‘to curette the lesion.’ The family was relieved and very grateful and wound up sending me a bunch of gifts.”
Dr. Maurer continued to lead the IRSG for 25 years. “We learned a lot about the disease,” he said. “We learned the pattern for how it spreads. For example, when we first started, there was a 100 percent mortality rate if it originated in the head and neck area and then spread to the brain. So, as soon as a tumor was identified in the head and neck region, we prophylactically treated the brain with radiation therapy. The survival rate soared.
“We developed a treatment regimen that involved radiation and a combination of three different chemotherapy drugs. It is still the gold standard for care today. By using this treatment regimen, we were able to eliminate the radical surgeries that were routinely done for rhabdomyosarcoma, such as amputation of a limb or removal of the orbit of the eye.”
The research grants continued to flow. Each year, the IRSG brought in about $1 million or more in research funding.
“Dr. (Tom) Rosenquist (vice chancellor of research) once told me that I had more research grants than any other researcher at UNMC,” Dr. Maurer said.
Although it’s been more than 10 years since Dr. Maurer conducted his research, he’s thrilled to see that the work of the IRSG is still remembered. Fittingly, in 2003, his illustrious research career was capped when the Children’s Oncology Group honored him with its prestigious Lifetime Achievement Award.