Three UNMC investigators are trying to save six million hearts.
That’s the number of people in the U.S. who suffer from chronic heart failure.
The trio of Irving H. Zucker, Ph.D., chairman, and professors Kaushik P. Patel, Ph.D., and Harold D. Schultz, Ph.D., are three of the world’s leading experts on heart failure. Together, they represent 124 years of research experience.
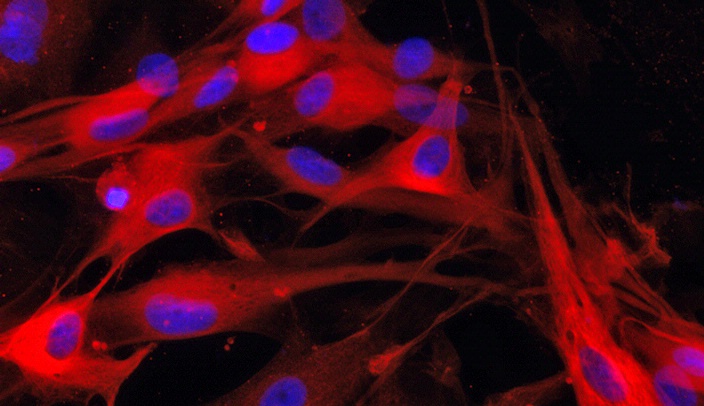
Dr. Zucker and his team in UNMC’s Department of Cellular and Integrative Physiology want to understand the pathophysiological processes that occur during the progression of chronic heart failure (CHF) with the hope of finding better treatment strategies to improve complications and longevity.
Specifically, they want to provide a comprehensive picture of how CHF augments the response, and enhanced response, of the sympathetic nervous system, which functions like a gas pedal in a car to trigger the body’s fight-or-flight response. To do so, the trio studies three different, but interrelated areas – the heart, brain and kidneys in CHF – and how exercise training affects these mechanisms.
They recently received their fourth, five-year renewal of a Program Project Grant (PPG), unprecedented at UNMC, worth more than $8 million to continue their research into how CHF augments the sympathetic neural function. They’ve been on this quest for the past 16 years.
“The heart is more than a muscle,” Dr. Zucker said. “It’s an intricate nervous system and it makes hormones. It’s not well appreciated because the focus is usually on its main function.”

Irving H. Zucker, Ph.D.
Heart failure has existed since the days of the Egyptian pharaohs, about 3,500 years ago, and despite the advancement of health care, it continues to be the No. 1 cause of death for men and women worldwide. In the U.S., the disorder annually claims more than 600,000 lives at a cost of more than $100 billion.
Nearly one-half of the deaths from heart disease are due to coronary ischemia that progresses to CHF, the most common diagnosis in hospitalized patients age 65 and older. About one-half of the people who develop heart failure die within five years of diagnosis.
The American Heart Association reports that between 2007 and 2010, 5.1 million Americans over the age of 20 suffered from this malady. By 2030, it is estimated that this number will increase by 25 percent.
The three investigators want to lower those numbers through exercise and new therapies – to provide options that go beyond current therapies that haven’t changed in 30 years.
Knowledge emerging from the PPG, which uses animal models of heart failure, has provided key insights into the neural and molecular mechanisms responsible for impaired autonomic control of the heart and kidneys during the progression of CHF.
The sympathetic nervous system controls unconscious functions of the body and is critical in the regulation of the heart and kidney. This neural system is regulated in at least two regions in the brain, the rostral ventrolateral medulla – a small region of the brainstem – and the paraventricular nucleus (PVN), which is located in the hypothalamus.
Determining the mechanism and therapeutic efficacy of exercise training has been one of the major goals of the grant and the team has demonstrated that exercise training, in animals, reverses the effects of CHF on the sympathetic nervous system.
Dr. Zucker’s team was one of the first to determine some of the mechanisms by which exercise training reduces sympathetic nerve activity in CHF.
Human studies show that exercise improves health 30 percent to 40 percent, and improves five-year survival rate of patients with CHF. Dr. Zucker has found that exercise training can reduce levels of a molecule – angiotensin II – that plays a key role in heart failure. His team was the first to show that angiotensin II leads to an increase in harmful free radicals in the brain during CHF.

Harold Schultz, Ph.D., and his research technician, Mary Ann Zink, look at an echocardiogram of heart failure in the left ventricle of a rat’s heart.
“In heart failure, the body experiences more oxidative stress that produces free radicals (the bad guys) and less antioxidants (the good guys),” Dr. Zucker said. “And these antioxidants aren’t the kind you get from eating blueberries.”
“We have found the origin of chemical changes in the hypothalamus and medulla – regions of the brain that mediate pre-sympathetic neuronal discharge,” Dr. Zucker said. “It’s a truly integrated system that jumps into sympathetic hyperdrive when heart failure occurs, and where exercise training can play a vital role.”
This integrated system between the heart, brain and kidneys also integrates the three projects in the PPG. The trio believes this is where they can find ways to turn molecular systems on and off to attenuate heart and kidney failure. The key may be two proteins they’ve discovered that act like ‘yin and yang’ during oxidative stress in the central nervous system.
“There is a novel relationship between proteins that promote oxidative stress and those that contribute to antioxidant effects,” Dr. Zucker said. One of the antioxidant transcription factors is called nuclear factor (erythroid-derived 2)-like 2 (Nrf2) and that’s what Dr. Zucker will study in his roject “Nrf2: Neuronal Oxidative Stress and Sympathetic Nerve Activity (SNA) in Heart Failure.”
“Figuring out how to activate Nrf2 may be critical to regulating that imbalance in the body,” he said. Dr. Zucker will try to “rescue” animals with CHF by overexpressing Nrf2 in the medulla.
“High oxidative stress occurs when Nrf2, an important promoter of antioxidant enzyme production, is deleted,” he said. “Other data indicates that deletion of this gene results in lower levels of antioxidant enzymes in areas of the brain that regulate SNA to the heart and blood vessels.”
He also is investigating how exercise training in rats with heart failure modulates oxidative stress through this interaction, and is extending previous studies on the role of central angiotensin converting enzyme 2 (ACE2) in activating Nrf2 to reduce oxidative stress.
“What this means for patients is still unclear,” he said, “but there are techniques that have been shown to increase Nrf2, such as exercise training.”
As CHF progresses, blood supply to tissues is reduced. Fluid regulation is compromised and the kidneys begin to retain salt and water. The resulting edema puts more stress on the heart.
For the past 30 years, Dr. Patel has been interested in the role of the PVN in the regulation of the circulation and renal function. In his project, “Activation of the PVN in Heart Failure: Role of HIF1-α, and Renal Afferents,” he studies the basic principles underlying intercellular communication between preautonomic PVN neurons to determine how changes within the PVN contribute to enhanced sympathetic drive in CHF.
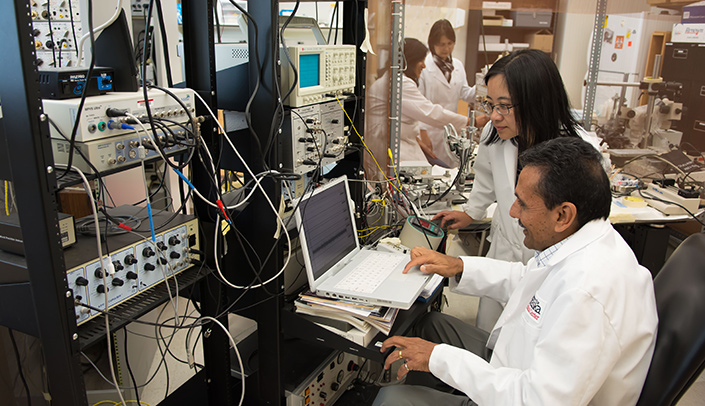
Kaushik Patel, Ph.D., and Hong Zheng, M.D., assistant professor, measure neurons in the brain. In the back, Neeru Sharma, Ph.D., assistant professor, shows Andrea Haibara, Ph.D., a visiting associate professor from the Federal University of Minas Gerais, Brazil, how to use a piece of equipment.
He also will explore the novel idea that sensory nerves originating in the kidney negatively influence neural control of circulation in CHF and contribute to that downward cycle of free radical production.
“Our theory is that if you cut renal nerves, you prevent this vicious cycle,” Dr. Patel said.
Then, there is the exercise component. “The hormones that control water and salt retention are the same that regulate blood pressure,” he said. “We have shown that exercise training allows for better function of the kidneys and improves the overall circulation and heart function.”
In the third project, “The Chemoreflex in Heart Failure,” Dr. Schultz explores the role of impaired blood flow on abnormal reflex control of the heart, kidneys and breathing in CHF.
“The problem of exercise with heart failure is that breathlessness limits exercise tolerance. Carotid body sensors mediate the sensation of breathlessness, or air hunger, which can impair exercise capacity,” Dr. Schultz said.
“The oxygen sensors in the carotid body become overly active in heart failure due to the inability of the failing heart to maintain adequate blood flow and oxygen delivery to the sensors. We are finding that selective interruption of this signal from the carotid body by surgical ablation or by exercise training improves breathing.”
Dr. Schultz’s work also has shown that abnormal carotid body stimulation increases sympathetic outflow to the kidney, which then increases salt and water reabsorption and an expansion of blood volume that the failing heart cannot adequately pump.
The project recently has shown that ablation of the carotid body improves the function of the kidneys and heart leading to greater survival in heart failure animals, which could have a translational impact for patients. Results from these studies have served as the basis for a recent ongoing clinical trial in humans.
Drs. Zucker, Patel and Schultz serve on numerous editorial boards of medical journals, lecture around the world and present papers to their peers. A small department by national standards, UNMC’s Department of Cellular and Integrative Physiology’s reputation stands tall internationally.
“Now when we stand up at meetings and say we’re from Nebraska, people know where that is,” Dr. Zucker said.
Web extra
Learn more about UNMC’s cardiovascular research.